Renee Davis was terrified to learn she had lung cancer. But White Plains Hospital’s excellent doctors — and its access to a cutting-edge clinical study — gave her hope for a cure.
It’s hard to imagine how a health emergency could turn out to be a positive. But that’s exactly what it was for Renee Davis, 67, a White Plains resident and supermarket clerk. Although her crisis was a severe allergic reaction, it uncovered another potentially deadly problem: lung cancer.
Davis’ journey began in late 2019, when, out of the blue, she felt an odd sensation on her face. “I looked at it in the mirror and thought, Holy smokes!” she recalls. “It was all swollen.” Soon, she began to have trouble breathing. She drove to urgent care and was sent immediately to White Plains Hospital’s Emergency Department, where she was admitted to the Intensive Care Unit. The physicians worked to stop the swelling and keep her airway open. Fortunately, after two days, she recovered. The likely allergen was identified as Davis’ blood pressure medication, and she was switched to a different drug.
Yet her worries weren’t over: the CT scan she received during treatment showed an unexplained mass. At a follow-up visit, she was directed to see Dr. Todd Weiser, the Hospital’s Director of Thoracic Surgery. Davis was understandably nervous, wondering what would come next, but as soon as she met Dr. Weiser, she felt she could trust him.
“He was so nice and didn’t speak to me like he was superior to me,” she says. He quickly arranged for Davis to have a PET-CT scan, which would provide more detailed information on the changes in her lungs.
What he saw was concerning. “The scan showed a large mass that was in the central part of her right lung, and the lymph nodes within her lung were enlarged,” Dr. Weiser says. He performed a lung biopsy as soon as possible, and it showed she had stage 2 lung cancer.
Davis was devastated by the news, but Dr. Weiser reassured her. “He told me he had my back and was going to do surgery to remove it,” she says. “Still, I went into the bathroom and fell to my knees. I wondered what I was going to tell my family. My older son was getting married in Mexico in July. I didn’t know if I’d be able to go to the wedding.”
Entering a Clinical Trial
The more immediate concern was to figure out what, in addition to surgery, would give Davis the best chance of a complete recovery. At Dr. Weiser’s recommendation, Davis met with Dr. Dan Costin, Director of the White Plains Hospital Center for Cancer Care, who proposed that she enter a clinical study on lung cancer treatment in which the Hospital was participating.
“It’s called Keynote 671,” Dr. Costin says. Participants, he explains, are divided into two groups. Both undergo chemotherapy before surgery rather than afterward, which is the standard treatment plan. In addition, during chemotherapy, half the patients receive immunotherapy, a treatment that helps the body’s immune system fight cancer. The other subjects receive a placebo.
The purpose of the study is to establish immunotherapy’s usefulness for treating lung cancer at earlier stages of diagnosis. “We know it works very well if you have very advanced or stage 4 lung cancer,” Dr. Costin says. “Renee’s cancer was at an early stage, but it’s a stage where, unfortunately, a significant number of patients are destined to have a recurrence, even when they’ve had surgery and standard chemotherapy.”
The trial, he told Davis, could potentially allow her to receive pembrolizumab, an immunotherapy drug that makes it difficult for cancer cells to hide from the immune system.
Despite knowing that the research project might give her access to cutting-edge treatment, Davis was hesitant. Her husband and two sons also had reservations, wondering if the experimental drug might have unforeseen health consequences.
“But then Dr. Costin explained it all to us during a visit,” Davis says. “He showed us photographs of different stages of cancer and explained why I was a very good candidate for the study and could potentially be helped a lot.” She and her family were convinced. “My older son said, ‘Mom, what do you have to lose?’”
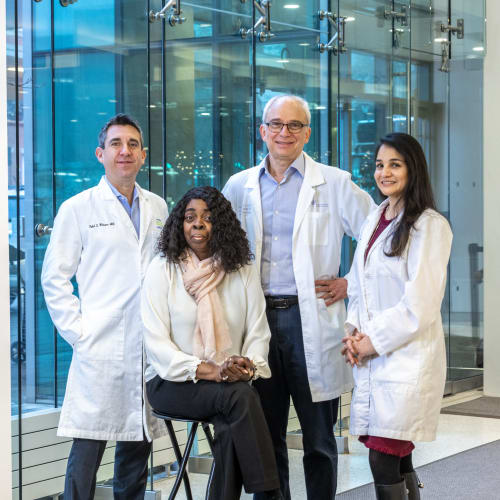
Renee Davis, center, with her care team at White Plains Hospital: Dr. Todd Weiser, Dr. Dan Costin, and Catherine Reilly, MPH, RN
The details of the study and treatment were further explained to Davis by Catherine Reilly, MPH, RN, a Clinical Research Nurse with the White Plains Hospital Center for Cancer Care. “I take care of patients who are enrolled in clinical trials,” Reilly explains. “In my initial discussions with them, we talk about the research study as a possible treatment option. I tell them about the purpose of the study and give them all the details. I also ensure that the patients meet the eligibility requirements for the clinical trial.
“In addition, at any given time, we have approximately 30 trials that are actively enrolling patients and other studies with patients in follow-up,” Reilly continues. The Hospital is playing a key role in the pembrolizumab study, she notes, as one of 42 other research sites worldwide. The fact that White Plains Hospital was selected to be part of this curated handful reflects its excellence, she adds.
“We have built a state-of-the-art, cutting-edge Cancer Center, and as part of it, we have invested in developing a strong clinical trials office with an outstanding director and an excellent supporting staff,” says Dr. Costin. “We have also been able to convey the importance of clinical trial participation to physicians and providers caring for our cancer patients. And we have an established oncology pharmacy with an interest and expertise in clinical research. As a result, our program has been very attractive when sites are being selected for clinical trials.”
Facing the Challenge Bravely
Davis began what would be the first of four IV treatments in January 2020. “The people at the infusion center were really nice. They treated me with such kindness,” she shares. But that wasn’t the only good news: Davis also felt no adverse effects from the chemotherapy and (possible) immunotherapy. She went into each infusion session with an upbeat attitude, even wearing fancy outfits a couple of times. “The nurses asked me where I was going, and I told them I just came here like that because I hadn’t worn those kinds of clothes in a while, so I thought I’d get dressed up,” she says.
All wasn’t cheerful, however. In March, just as Davis was preparing for her third infusion, the pandemic began. “Suddenly, we were in a situation where we were wondering if we could even bring our patients in to get standard chemotherapy, let alone if they were in clinical studies,” Dr. Costin says. However, White Plains Hospital took every possible step to make sure non-COVID patients were kept safe, and Davis still got the attention she needed. “We placed her on high priority. She never missed a treatment,” Dr. Costin explains.
The results of the infusions were astonishing. Screenings showed Davis’ tumor, which had originally measured more than 2.5 inches, had been completely eradicated. Although she and Dr. Costin don’t know if she received immunotherapy or the placebo, the malignancy “literally melted away, which would be very unusual if you were getting chemotherapy alone,” he says. “We suspect that she got pembrolizumab, but either way, she had a terrific response. And this is why clinical studies are so important, because they’re entering into the frontier.”
Sweet Victory
In May 2020, Davis had surgery to remove the last, tiny traces of her cancer. She was nervous, but Dr. Weiser had long ago won her confidence. “I told him I was going to put my trust in him, and I wanted him to understand that I’d already asked God to guide his hands,” she says.
Using minimally invasive techniques, Dr. Weiser took out the lingering remnants of the malignancy, an area which measured only a couple of millimeters. “There was no residual tumor in something that had once been the size of a golf ball,” Dr. Weiser notes. He removed several lymph nodes for testing, as well, and they were cancer-free. “Renee did great with the surgery,” he says, adding that she returned home after just three days.
Dr. Costin gave Davis maintenance medication to further minimize the risk of a recurrence. She finished the regimen in March of 2021. “I would tell anyone in my situation to go to White Plains Hospital,” Davis says. “I thank God every day that I’m alive.”
She was especially grateful that she was able to attend her son’s wedding. “I thought, I made it!” she shares. It was a cherished chance to see her son begin a new, happy chapter of his life — while she began a new, healthy chapter of her own.
To learn more about White Plains Hospital's Center for Cancer Care, visit wphospital.org/cancer
