White Plains Hospital now offers the Barricaid Spine Treatment, a herniated-disc repair that reduces the largest risk factor in discectomy surgery.
Patients who struggle with sciatica, or leg pain, can often trace the discomfort to a herniated disc in their lower back. You don’t have to be a powerlifter to be at risk for a herniation; sometimes it’s just a result of normal wear and tear. Nestled between each of the vertebrae in the spinal column is a disc with a soft, jellylike center (nucleus pulposis) ringed by a firmer, rubbery border (annulus). When that squishy center protrudes through a weakened spot in the annulus, it feels anything but cushy. In fact, the pressure it exerts upon nerve roots in our spine can cause weakness, numbness, or pain intense enough to require surgery. But that repair, called a discectomy, has one major drawback: the annular ring could possibly tear again before it completely heals. That scenario, called reherniation, is a source of frustration to both the surgeon and the patient and typically results in more surgery.
New Approach
But what if a breakthrough could end the uncertainty and aggravation? “Until now, most medical advances in orthopedic and spine surgery have been variations on the same theme. Barricaid, however, is a novel concept,” says Dr. Jared Brandoff, Orthopedic Surgeon at White Plains Hospital Physician Associates. “We can surgically remove the protruding or extruded fragments compressing the nerves in the spinal canal, which relieves pain. However, the body has to mend the hole in the annulus on its own, over time. In that time, reherniation can occur. Reherniation is not anybody’s fault; it’s just bad luck.”
 Dr. Jared Brandoff is an Orthopedic Surgeon at White Plains Hospital Physician Associates.
Dr. Jared Brandoff is an Orthopedic Surgeon at White Plains Hospital Physician Associates.
And because the spine is constantly recruited to help us move — bending, reaching, lifting, even simply maintaining posture — it remains vulnerable to ruptures, which can send patients back to square one. In fact, one in three patients who receive a discectomy still has significant weakness in the outer rim of the ruptured disc.
“We needed a way to plug the hole to prevent reherniations from occurring,” says Dr. Brandoff. When he heard about an FDA-approved, boneanchored implant recently introduced in the United States, he sought training immediately. This year, Dr. Brandoff was the first surgeon in Westchester County to perform the Barricaid Spine Treatment procedure. Tinier than a pencil eraser, the Barricaid implant has a polymer barrier that slips into the disc to block the hole, paired with a titanium anchor affixed to the bone.
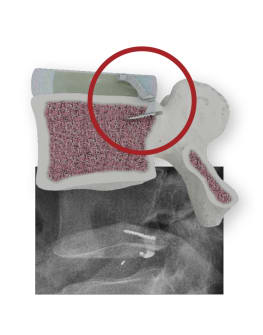 The Barricaid implant inserted into a disc and on X-ray.
The Barricaid implant inserted into a disc and on X-ray.
“With this device, we’re reducing the risk of reherniation by 80 percent,” says Dr. Brandoff. “This is a truly novel solution that addresses what used to be an unavoidable complication of surgery.” With the hole sealed, patients can begin the healing process without the threat of another herniation — resulting in a faster and easier recovery.
Who can benefit?
Good candidates for the Barricaid procedure are active, healthy patients with disc herniations in their lower backs and without severe arthritis, Dr. Brandoff explains. He consults X-rays and MRIs to study the shape and size of the herniated disc and severity of the canal narrowing. “Repeated operations for herniated discs can cast a long shadow over patients whose pain has already interrupted their lives,” he says. “The Barricaid procedure offers healing — and hope.”
To make an appointment at White Plains Hospital's Center for Orthopedic & Spine Surgery, call 914-849-7897.
