Image above from left: Drs. Heidi Wang, Charles Noyer, Melissa Magrath, and Mukul Arya. Missing from the photo: Dr. Philip Weber
White Plains Hospital’s new Esophageal Program brings together multi-disciplinary experts to care for patients with a variety of swallowing and digestive conditions.
Problems with your esophagus, the muscular tube that moves food from the mouth to the stomach, can be more than annoying; they can take over your life. Depending on the particular condition, you can experience anything from frequent heartburn to difficulty swallowing food, making eating a chore instead of a joy.
One common issue is severe gastroesophageal reflux disease, or GERD, which is when stomach acid flows back into the esophagus. It’s linked to obesity and other factors, such as diet, and 15% of the population experiences it. Yet despite how common it is, it’s often difficult to pinpoint the problem since GERD symptoms, such as coughing and nausea, are also associated with other conditions.
Getting an accurate diagnosis and proper treatment for GERD and other esophageal disorders has been a challenge —until now. White Plains Hospital’s new Esophageal Program, which launched six months ago, offers a comprehensive approach to complex conditions. It combines the latest technology and treatments with experienced White Plains Hospital gastroenterologists and surgeons to provide a coordinated team approach to care. The program’s experts — Drs. Melissa Magrath, Charles Noyer, Heidi Wang, and Philip Weber — not only work together closely, but also have offices proximate to one another’s, ensuring comprehensive care.
Robotics and Bariatrics at White Plains Hospital
“We have all treated these conditions for many years, but new advancements in technology, along with minimally invasive and non-surgical procedures, have allowed us to create an innovative multispecialty offering for our patients,” says Dr. Philip Weber, Director of Minimally Invasive Surgery, Robotics and Bariatrics at White Plains Hospital. “We have streamlined this program so that when you come in you will see everyone involved in your care and you will leave with your questions answered and a plan for next steps.”
Extensive Testing Options
While some patients who come to the program have already been diagnosed with an esophageal condition, others require specialized testing to determine their issue. For that they see Dr. Magrath, a board-certified gastroenterologist with the Hospital who specializes in this area. One particularly helpful diagnostic procedure she performs is called a Bravo test. “It’s a wireless acid reflux test,” she explains.
The process to test for GERD is fairly straightforward: while sedated, a patient undergoes an endoscopy, a nonsurgical procedure that uses a flexible tube with a camera and light to examine the esophagus, stomach, and the first part of the small intestine. Dr. Magrath then attaches a very small clip to the esophageal wall. Patients carry a small electronic device for four days that wirelessly transmits information about what percentage of the day the wearer is experiencing reflux.
“The patients can also tell us when they have heartburn by pressing buttons on the recorder. The computer gives us data on whether it is correlated to the time the person is having reflux,” Dr. Magrath explains. Eventually, the chip falls away on its own and is passed through the body painlessly.
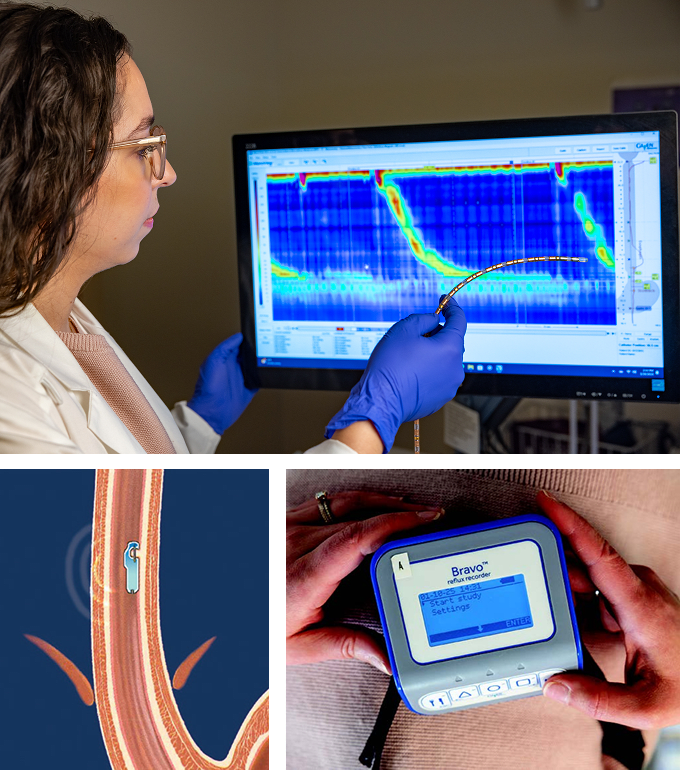
The test is far more accurate than an endoscopy performed without a chip and recording system, since such tests only examine the patient’s condition during the exam. “70% of people will have a completely normal endoscopy,” Dr. Magrath says, “but monitoring the patient for four days can provide proof of reflux as well as information that can help determine whether a patient needs medication or surgery.”
Surgical and Non-Surgical Treatment Options
It is important to treat GERD, as it can lead to complications. If stomach acid gets into the throat or windpipe, it can bring on asthma in people who have that condition. GERD can also cause a chronic cough, cardiac and sinus issues, and even the loss of tooth enamel due to erosion caused by the acid.
Once someone is diagnosed with chronic reflux, there are several treatment options available. In some cases, medication alone may help, however, these medications may not be right for everyone.
A Non-Surgical Reflux Fix
If a patient’s acid reflux test is positive and they are interested in an anti-reflux procedure, they generally see one of the other experts in the program. Dr. Charles Noyer, Director of Gastroenterology at White Plains Hospital, is among them.
Sometimes, Dr. Noyer explains, GERD is caused when acid from the stomach washes up into the esophagus due to a damaged or worn-away valve between the two. In that case, the patient can benefit from a TIF procedure. “It stands for ‘transesophageal incisionless fundoplication.’ Because no incisions are made, it is not considered a surgery,” Dr. Noyer explains.
During the procedure, the patient is placed under anesthesia. Using an endoscope, Dr. Noyer then places a device where the valve ought to be, recreating the barrier between the stomach and the esophagus. To complete the procedure and create a tight seal, he creates a new valve at the junction of the stomach and the esophagus and inserts special plicators—small devices that fold and secure tissue—to keep it intact. No scars are created.
Hernia Repair
Sometimes, a patient’s reflux isn’t related to their esophageal valve, or the esophageal valve isn’t only to blame. Instead, the problem may be due to an issue called a hiatal hernia, A hiatal hernia is a widening of the diaphragm muscles where the esophagus connects to the stomach. When this opening is enlarged, part of the stomach or other organs in the abdomen can push up into the chest cavity.
“When this happens, we want to first restore the stomach or other organs back into the abdomen, then close the diaphragm snugly around the esophagus,” explains Dr. Heidi Wang, a surgeon in the program who specializes in the repair of hiatal hernias. To do so, she must tighten the seal around the esophagus. Amazingly, this surgery is performed laparoscopically, requiring only small incisions in the patient to insert a camera for an internal view.
Very gently, Dr. Wang pushes the stomach back down below the diaphragm. Next, she addresses the hernia, sometimes using robotic arms to assist her. “Using sutures, we close up the hole around the esophagus and create a tight ring around it,” Dr. Wang says. If necessary, Dr. Noyer then performs the TIF procedure.
Help for Problems with Swallowing
In addition to testing patients for reflux, Dr. Magrath also diagnoses patients who complain that they have trouble swallowing and food gets stuck in their esophagus. This problem can be due to a rare disorder called achalasia. In patients with this issue, the esophagus muscles don’t properly move food along, and a ring-shaped muscle called a sphincter, located at the bottom of the esophagus, doesn’t relax to let food pass to the stomach. When this occurs, it can lead to symptoms of food regurgitation and chest pain with eating. People with achalasia may find eating to be uncomfortable, and eventually start to lose weight.
Dr. Mukul Arya, Director of Advanced Gastroenterology at White Plains Hospital, is an expert in achalasia repair, and a key member of the Esophageal Program. To fix the problem, he performs a nonsurgical procedure called per oral endoscopic myotomy, or POEM for short. Using an endoscope inserted through the mouth, he makes several cuts in the esophagus and upper stomach, which allow food to pass easily. Recovery is so easy that the patient can go home the next day. Afterward, they are periodically monitored.
“We follow up to make sure that their symptoms are gone, patients are eating regularly, and they are gaining weight,” Dr. Arya says.
A True Team Effort
White Plains Hospital’s Esophageal Program offers help in a coordinated way. “Patients know we are collaborating on their care,” Dr. Magrath notes.
“I’ve heard a lot from patients that it’s really hard to get their doctors to talk to each other when it’s necessary to collaborate, but in our program it’s easy for doctors to communicate with each other and with the patient,” she continues. The public reception to the program has been extremely enthusiastic. “We can really help our patients,” Dr. Magrath says. “We pinpoint their diagnosis and provide the treatment they need to enhance their quality of life.”
Don't suffer from GERD any longer. Learn more about White Plains Hospital’s Esophageal Program or call 914-948-1000 to make an appointment.
